Posted: October 14, 2012
The National Disaster Medical System Federal Partners Memorandum of Agreement defines a public health emergency as "an emergency need for health care [medical] services to respond to a disaster, significant outbreak of an infectious disease, bio terrorist attack or other significant or catastrophic event. For purposes of NDMS activation, a public health emergency may include but is not limited to, public health emergencies declared by the Secretary of HHS [Health and Human Services] under 42 U.S.C. 247d, or a declaration of a major disaster or emergency under the Robert T. Stafford Disaster Relief and Emergency Assistance Act (Stafford Act), 42 U.S.C. 5121-5206)."
The Act has provisions for infectious diseases that have the potential to threaten national security by incapacitating public employees, the military, etc. It does not have a provision for multi-state iatrogenic (man made) non infectious events such as the fungal meningitis outbreak. While “covered events” such as an outbreak of swine flu trip the coordination of specific public responses, “noncovered events” such as this outbreak of fungal meningitis rely on individual states to determine their own response systems. The risks associated with the event are transferred to the individual, affording them little or no protection beyond existing regulation.
Where tracking has occurred, an effort has been made to track from the clinic level to the consumer wherever they may be located. Consumers who reside in other states have been directed to their resident state departments of public health for information. If the state has not been notified that clinics in their jurisdiction received contaminated materials, they have not stood up a statewide response. Consumers in the opportunity threat zone cannot find their way to adequate information within their functional treatment zone. That’s a problem. It appears that at this time, the best way to find information is through the department of public health for the state in which you received treatment.
Because a multistate coordinated response has not been put into place, we are observing a host of predictable problems that increase the difficulty for individual affected consumers:
Barriers to recall at the physician practice level – Consumers are reporting that medical practitioners did not track the information necessary for an effective recall. Medical records do not reflect the necessary information about dosage, product, and lot code. Dosage vials may have been used across multiple consumers and traceability is non existent. Phyisician procurement systems lack identifying information, product specifications are missing, ingredient declarations are absent, lot tracking numbers are not codified into inventory management. Consumer records may be incorrect or incomplete. In some cases, consumers received contaminated injections after the national recall was issued on September 25, leading providers to conclude incorrectly that injections issued after that date are not covered by event procedures.
Barriers to care – Because rimary care is separated from pain management and emergency response, another layer of complexity is added to the process. Local hospitals are responding inconsistently to individuals who present with symptoms. In some cases, physicians are refusing to treat due to fear of personal litigation. It may be difficult for individuals to resolve the payor responsibility issues, particularly where the originating treatment arises from a workman’s compensation injury but the person is affected by a secondary injury due to exposure to contaminated materials. Treating to the limits of personal insurance plans promotes wide variation in treatment response. Where diagnostic procedures require prior authorization or the fungal medications are not approved for payment, those costs will be passed on to the consumer. This creates immediate access to care issues
In some states, physician practices routinely charge patients for copies of their records and may refuse to release health records without a hefty fee. While many of use maintain emergency contacts, this is not the same as a designated care partner who can act on our behalf when we are incapacitated. Someone who is acknowledged with the right to become actively involved in treatment decisions must be sorted out in the middle of the crisis.
Evaluate this in terms of who is affected by the outbreak
Most of the affected are already affected by disabling levels of chronic pain which already limits personal resources for response. While some of their pain events may have originated in a work place accident, for many, a long standing battle with chronic pain is reflected in their histories. Already disadvantaged, this man made emergency will result in adding insult to injury on many levels. It is important to understand this event in terms of the system in which it has occurred and the layers of failure that resulted in personal injury on a wide scale.
This article was written by an citizen health care advocate Terri Lewis. She is not an attorney. With so many lawyers out there seeking fungal meningitis cases sometimes critical issue fly under the radar and points of view that demand systematic changes are missed.
Terri is a Doctoral Candidate in Rehabilitation Counseling and Administration at SIU-C, a trained Red Cross responder, a researcher, and a subject matter expert in issues that result in health care failure for persons with chronic pain that originates with spinal chord injury. She has extensive experience in community health care integration, public policy and ethics. Terri collaborates with worldwide consumer communities of care and research communities of practice.
Related Posts:
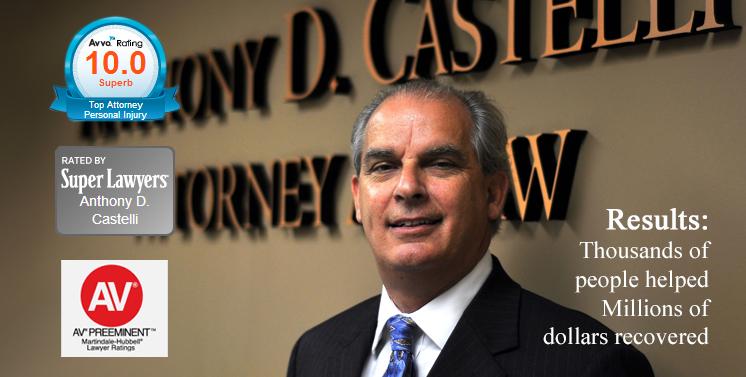
Anthony Castelli Attorney is focusing on helping victims of this fungal meningitis outbreak and long term preventatitve measures. Anthonyis investigating his belief that there may be many negligent parties as this crisis is deeper and wider than just NECC.